Cardiac tumors (cardiac neoplasms)
Cardiac tumors may be primary (benign or malignant) or metastatic (these are always malignant and are far more common than primary tumors). Signs and symptoms are nonspecific and highly variable depending on the localization, size, and composition of the cardiac neoplasm. The first imaging modality alerting the clinician to the presence of a cardiac mass usually is echocardiography, most often performed for another indication.Primary tumors of the heart
Primary cardiac tumors are rare. They are much rarer than metastatic ones. Most primary cardiac tumors are benign (75-80%). The most common type of primary benign cardiac tumor is myxoma (followed by lipoma and fibroelastoma).Primary malignant cardiac tumors are extremely rare and they are almost all sarcomas, with angiosarcoma being the most common among them (Lymphomas and malignant paragangliomas are even more rare types of primary cardiac malignancies). Sarcomas can occur in any chamber of the heart but they are more frequently located in the right or left atrium. Malignant cardiac tumors have a poor prognosis.
In childhood, primary cardiac tumors are extremely rare and mainly include rhabdomyoma and fibroma. Rhabdomyomas are the most common cardiac tumors in childhood. Cardiac rhabdomyomas are benign tumors that originate from cardiac myocytes. Some cases are sporadic and isolated, but in 50% of cases, they are associated with tuberous sclerosis. The most common malignant cardiac tumor in childhood is rhabdomyosarcoma. Cardiac tumors in children are often associated with genetic syndromes.
Primary cardiac tumors should be totally resected (in a cardiac operation performed on cardiopulmonary by-pass) whenever possible. For benign cardiac tumors, this is almost always possible.
The perioperative mortality is about 8% overall but for myxoma, which is the most common cardiac tumor resected, the perioperative mortality is much lower, approximately 1% .
Metastases to the heart can occur by the following three mechanisms:
The site of the heart most commonly affected by metastatic malignant disease is the pericardium. Pericardial involvement results in a pericardial effusion which is often large and hemorrhagic and may contain masses comprising of cancer cells or blood clots and fibrin. Thus, echocardiography apart from the echolucent pericardial effusion may demonstrate distinct regions of thickening of the visceral pericardium. Generally, pericardial metastases are common and they result in persistent pericardial effusions, also posing the risk of tamponade. The differential diagnosis in a patient with known malignant neoplasm and a pericardial effusion includes malignant pericardial effusion (metastasis to the pericardium), radiation-induced pericarditis, drug-induced pericarditis, and idiopathic pericarditis. In many cases, a histologic diagnosis can be made by pericardial fluid aspiration or pericardial biopsy. Treatment with a pericardial window and/ or fibrosing agents lessen the need for repeated pericardiocentesis.
The perioperative mortality is about 8% overall but for myxoma, which is the most common cardiac tumor resected, the perioperative mortality is much lower, approximately 1% .
Metastatic cardiac tumors
Metastatic cardiac tumors are far more frequent (approximately 30- 40 times more frequent) than primary tumors of the heart. Neoplasms that may involve the heart are mainly melanomas, lymphomas, lung, breast, and renal cancer.Metastases to the heart can occur by the following three mechanisms:
- Direct extension of a neoplasm via adjacent tissues
- Dissemination of cancer cells in the blood or the lymphatic system
- Propagation through the superior or the inferior vena cava to the right atrium.
Less often metastatic tumors may affect the myocardium or the endocardium (causing manifestations of heart failure or arrhythmias), or the venae cavae (causing manifestations due to obstruction of venous flow). Generally, possible presentations of a myocardial metastasis include nonspecific ST-T wave changes, cardiac arrhythmias, heart block, or myocardial dysfunction.
Echocardiography is the most commonly used imaging method in suspected cardiac metastatic disease, but magnetic resonance imaging and computed tomography are also valuable. Metastatic tumors affecting the myocardium, usually appear as distinct, brightly echogenic masses. Rarely, metastatic tumors may seed the endocardium and echocardiographically appear as intracavitary masses.
Cardiac metastases are clinically apparent only in 10% of the cases, and usually, they are not the cause of the patient's presenting symptom, although in some cases they cause symptoms (dyspnea due to heart failure, or due to a large pericardial effusion, chest pain due to pericarditis, signs of cardiac tamponade, arrhythmias, syncope due to atrioventricular block, etc). They usually occur in the setting of a previously diagnosed malignant neoplasm ( almost always a widespread primary neoplasm). The differential diagnosis of a cardiac manifestation in a patient with cancer includes cardiotoxicity because of chemotherapy or occurrence of cardiac metastases.
The general prognosis of patients with cardiac metastases is poor. For patients with intramyocardial metastasis, survival generally is limited to a few months at most. Survival is longer for intracavitary tumors. Occasional patients have survived several years.
Symptoms and signs of cardiac tumors are related to obstruction of blood flow, embolic phenomena, pericardial involvement, cardiac failure, arrhythmias and elaboration of substances causing constitutional symptoms. Since embolic and obstructive phenomena are common, the presenting symptoms of cardiac tumors are generally more related to their location in the heart and their size and less to the tumor type.
Myxomas, as well as other primary cardiac tumors, may present with one or more of a classic triad of manifestations which includes sequelae of valvular obstruction, embolic phenomena and constitutional symptoms.
Manifestations of heart failure are common in case of large intracavitary tumors causing obstruction to blood flow. Depending on the heart chamber involved, the resulting manifestations may be of :
Intracardiac (intracavitary) tumors, if they are large enough, cause clinical manifestations due to the obstruction of blood flow. Myxomas of the left atrium may prolapse via the mitral valve, causing symptoms of mitral obstruction (dyspnea, syncope depending on a change of patient's position, etc.). Tumors of the right heart chambers may manifest with signs and symptoms of right-sided heart failure. Primary malignant cardiac tumors can also cause congestive heart failure when there is extensive myocardial involvement.
Constitutional symptoms (fever, chills, fatigue, malaise, weight loss, Raynaud phenomenon), as well as some laboratory findings (elevated erythrocyte sedimentation rate, anemia, polycythemia, leucocytosis, thrombocytosis, thrombocytopenia), result from substances secreted by the tumor or released due to tumor necrosis.
The constitutional symptoms, signs and laboratory findings may resemble the findings of vasculitis or autoimmune connective tissue disease.
Embolism due to a cardiac tumor can in many cases be the first manifestation. An embolism can manifest as a pulmonary embolism or more commonly as a peripheral embolism (e.g a stroke or acute ischemia of an extremity or a digit), depending on the location of the tumor in a right or left heart chamber, respectively. The embolus consists either of tumor cells or of thrombi formed on the tumor surface.
Atrial or ventricular arrhythmias or atrioventricular block can occur as a result of tumor infiltration of the myocardium or the conductive pathways of the heart. This is particularly true for fibromas (these are intramural tumors, located in the left ventricle, mainly in the interventricular septum). In some cases, sudden cardiac death is the first manifestation of a cardiac tumor.
The clinical examination is nonspecific in cardiac tumors. However, cardiac symptoms and signs in a patient who has had no previous cardiac disease, in association with general symptoms and embolic events, should initiate cardiac investigations.
Differential diagnosis of an intracavitary cardiac tumor includes an intracavitary thrombus. Contrast injection can be helpful in the differential diagnosis because it will intensify the signals from tumors, but not from thrombi.
If echocardiographic findings cannot suggest the diagnosis, further imaging procedures such as computed tomography (CT) or magnetic resonance imaging are employed. Magnetic resonance imaging (MRI) provides the best spatial resolution and allows exact localization of the tumor. It may also differentiate fat from a thrombus or tumor. It provides particularly valuable information for intramyocardial and malignant tumors.
In differentiating between benign and malignant neoplasms, a useful test is18F-fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT). If there is a decision to proceed with cardiac tumor surgery (surgical excision of the tumor under cardiopulmonary by-pass), in the presence of risk factors for coronary heart disease, coronary angiography or CT coronary angiography should be performed, so that coronary stenoses can be bypassed during surgery for the tumor. Note that primary cardiac tumors should be totally resected whenever possible.
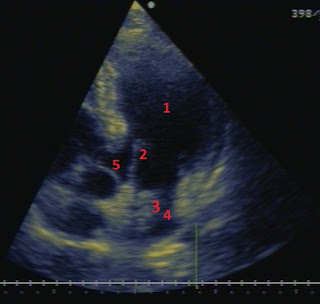
A woman 55 years old with a history of diabetes and hypertension. The ECG showed sinus rhythm with mild nonspecific T wave inversion. Recently she suffered an ischemic stroke with mild left hemiparesis. A 5-chamber apical echocardiographic view of this patient is shown below. Please name the structures 1-5. What has probably caused the ischemic stroke and which is the proposed management ?
1. Left ventricle 2. Mitral valve 3 A mass in the left atrium, with an appearance which is highly suggestive of a tumor (with a myxoma being by far the most probable diagnosis). A thrombus could be considered in the differential diagnosis, but in this case, it is not likely since there is a left atrium of normal size, and there was no history of atrial fibrillation or of mitral stenosis (conditions that can lead to the formation of a left atrial thrombus). Also, the position and size of the mass are clearly more suggestive of a tumor than of a thrombus. 4. Left atrium 5. Aorta.
The patient was managed with a successful surgical resection of the tumor. Biopsy has proven that it was a myxoma.
GO BACK TO THE HOME PAGE AND TABLE OF CONTENTS LINK :
CARDIOLOGY BOOK ONLINE-HOME PAGE AND TABLE OF CONTENTS
Paraskevaidis IA, Michalakeas CA, Papadopoulos CH, Anastasiou-Nana M. Cardiac Tumors. ISRN Oncology 2011:1-5. http://dx.doi.org/10.5402/2011/208929
Hoffmeier, A, Sindermann, JR, Scheld H, Martens, S. Cardiac Tumors-Diagnosis and Surgical Treatment. Deutsches Ärzteblatt International 2014; 111: 205-211. http://doi.org/10.3238/arztebl.2014.0205
Takahashi A, Otsuka H, Harada M. Multimodal Cardiovascular Imaging of Cardiac Tumors. 2015;2(1):61-67. http://dx.doi.org/10.17996/anc.02.01.61
Mankad R, Herrmann J. Cardiac tumors: echo assessment. Echo Res Pract 2015;3(4):R65-R77. http://dx.doi.org/10.1530/erp-16-0035
Echocardiography is the most commonly used imaging method in suspected cardiac metastatic disease, but magnetic resonance imaging and computed tomography are also valuable. Metastatic tumors affecting the myocardium, usually appear as distinct, brightly echogenic masses. Rarely, metastatic tumors may seed the endocardium and echocardiographically appear as intracavitary masses.
Cardiac metastases are clinically apparent only in 10% of the cases, and usually, they are not the cause of the patient's presenting symptom, although in some cases they cause symptoms (dyspnea due to heart failure, or due to a large pericardial effusion, chest pain due to pericarditis, signs of cardiac tamponade, arrhythmias, syncope due to atrioventricular block, etc). They usually occur in the setting of a previously diagnosed malignant neoplasm ( almost always a widespread primary neoplasm). The differential diagnosis of a cardiac manifestation in a patient with cancer includes cardiotoxicity because of chemotherapy or occurrence of cardiac metastases.
The general prognosis of patients with cardiac metastases is poor. For patients with intramyocardial metastasis, survival generally is limited to a few months at most. Survival is longer for intracavitary tumors. Occasional patients have survived several years.
Symptoms and clinical findings of cardiac neoplasmatic disease
Symptoms and signs of cardiac tumors are related to obstruction of blood flow, embolic phenomena, pericardial involvement, cardiac failure, arrhythmias and elaboration of substances causing constitutional symptoms. Since embolic and obstructive phenomena are common, the presenting symptoms of cardiac tumors are generally more related to their location in the heart and their size and less to the tumor type.
Myxomas, as well as other primary cardiac tumors, may present with one or more of a classic triad of manifestations which includes sequelae of valvular obstruction, embolic phenomena and constitutional symptoms.
Manifestations of heart failure are common in case of large intracavitary tumors causing obstruction to blood flow. Depending on the heart chamber involved, the resulting manifestations may be of :
- congestive (backward) heart failure, such as dyspnea, peripheral edema, or
- low cardiac output (forward) heart failure, such as fatigue, or hypotension.
Intracardiac (intracavitary) tumors, if they are large enough, cause clinical manifestations due to the obstruction of blood flow. Myxomas of the left atrium may prolapse via the mitral valve, causing symptoms of mitral obstruction (dyspnea, syncope depending on a change of patient's position, etc.). Tumors of the right heart chambers may manifest with signs and symptoms of right-sided heart failure. Primary malignant cardiac tumors can also cause congestive heart failure when there is extensive myocardial involvement.
Constitutional symptoms (fever, chills, fatigue, malaise, weight loss, Raynaud phenomenon), as well as some laboratory findings (elevated erythrocyte sedimentation rate, anemia, polycythemia, leucocytosis, thrombocytosis, thrombocytopenia), result from substances secreted by the tumor or released due to tumor necrosis.
The constitutional symptoms, signs and laboratory findings may resemble the findings of vasculitis or autoimmune connective tissue disease.
Embolism due to a cardiac tumor can in many cases be the first manifestation. An embolism can manifest as a pulmonary embolism or more commonly as a peripheral embolism (e.g a stroke or acute ischemia of an extremity or a digit), depending on the location of the tumor in a right or left heart chamber, respectively. The embolus consists either of tumor cells or of thrombi formed on the tumor surface.
Atrial or ventricular arrhythmias or atrioventricular block can occur as a result of tumor infiltration of the myocardium or the conductive pathways of the heart. This is particularly true for fibromas (these are intramural tumors, located in the left ventricle, mainly in the interventricular septum). In some cases, sudden cardiac death is the first manifestation of a cardiac tumor.
The clinical examination is nonspecific in cardiac tumors. However, cardiac symptoms and signs in a patient who has had no previous cardiac disease, in association with general symptoms and embolic events, should initiate cardiac investigations.
Diagnosis of cardiac tumors
Whenever a cardiac mass is encountered on echocardiography, the differential diagnosis includes a thrombus, a vegetation or a tumor, with the first two being much more common in comparison with a tumor. To reach a conclusion the physician should focus on:- the clinical context and presentation
- the location
- the imaging characteristics
- the findings of additional imaging tests (when necessary), such as CT or MRI
- in case of a tumor the definitive diagnosis is by biopsy (histological examination), although imaging is in many cases suggestive of the correct diagnosis.
Differential diagnosis of an intracavitary cardiac tumor includes an intracavitary thrombus. Contrast injection can be helpful in the differential diagnosis because it will intensify the signals from tumors, but not from thrombi.
If echocardiographic findings cannot suggest the diagnosis, further imaging procedures such as computed tomography (CT) or magnetic resonance imaging are employed. Magnetic resonance imaging (MRI) provides the best spatial resolution and allows exact localization of the tumor. It may also differentiate fat from a thrombus or tumor. It provides particularly valuable information for intramyocardial and malignant tumors.
In differentiating between benign and malignant neoplasms, a useful test is18F-fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT). If there is a decision to proceed with cardiac tumor surgery (surgical excision of the tumor under cardiopulmonary by-pass), in the presence of risk factors for coronary heart disease, coronary angiography or CT coronary angiography should be performed, so that coronary stenoses can be bypassed during surgery for the tumor. Note that primary cardiac tumors should be totally resected whenever possible.
A woman 55 years old with a history of diabetes and hypertension. The ECG showed sinus rhythm with mild nonspecific T wave inversion. Recently she suffered an ischemic stroke with mild left hemiparesis. A 5-chamber apical echocardiographic view of this patient is shown below. Please name the structures 1-5. What has probably caused the ischemic stroke and which is the proposed management ?
1. Left ventricle 2. Mitral valve 3 A mass in the left atrium, with an appearance which is highly suggestive of a tumor (with a myxoma being by far the most probable diagnosis). A thrombus could be considered in the differential diagnosis, but in this case, it is not likely since there is a left atrium of normal size, and there was no history of atrial fibrillation or of mitral stenosis (conditions that can lead to the formation of a left atrial thrombus). Also, the position and size of the mass are clearly more suggestive of a tumor than of a thrombus. 4. Left atrium 5. Aorta.
The patient was managed with a successful surgical resection of the tumor. Biopsy has proven that it was a myxoma.
--------------------------------------------------------------------------------------------------------------------------
Is there any abnormality in this image of cardiac magnetic resonance imaging (MRI)?
Name the structures shown in the image.
There is a large intracavitary mass in the left ventricle in contact with the apical part of its lateral wall which has a morphology suggestive of a cardiac tumor. The mass is homogeneous, broad-based and well circumscribed. 1. left ventricle 2 interventricular septum 3 right ventricle 4 tumor in the left ventricle 5 left atrium 6 mitral valve 7 right atrium. 8 intratrial septum 9 left lung 10 right lung. 11 descending aorta. The mass was surgically excised and histologic examination showed that it was a lipoma (left ventricular lipoma) Note that transverse sections in MRI or CT are displayed as if the viewer looks at the patient from the patient's feet, so that the left-sided structures are seen on the right side of the image , the right-sided structures on the left side of the image, the anterior structures are seen on the top of the image and the posterior structures on the bottom. Courtesy of Dr. Ketikoglou Dimitrios, Cardiologist MD PhD FESC
-------------------------------------------------------------------------------------------------------------------------
A patient with hepatic cancer. What kind of view is this, how is it obtained, which are the structures 1-6 and what is the probable diagnosis for this patient ?
This is a transesophageal echocardiographic (TEE) bicaval view (a long axis view of the right atrium obtained from the middle esophageal position with a plane angle of about 90-100oand clockwise rotation of the transducer shaft). 1 left atrium 2 interatrial septum 3 entrance of the superior vena cava, 4 right atrium 5 entrance of the inferior vena cava 6 a large non-homogeneous mass in the right atrium with a morphology suggestive of a tumor. It is a metastatic tumor from the liver (as suggested by the patient's history which has metastasized through a hepatic vein and then through the inferior vena cava into the right atrial cavity. Courtesy of Dr. Ketikoglou Dimitrios, Cardiologist MD PhD FESC
A 3-D echocardiographic image. Which view is this and where is the abnormality ? Name possible symptoms that may result from such a pathology.
An apical 4-chamber 3-dimensional echocardiographic view showing a mass (tumor) in the left atrium. This was a rare case of metastasis of a tumor of the small intestine. A tumor in the left atrium can cause dyspnea (due to elevated left atrial and pulmonary venous pressure), syncope, arterial embolism (e.g. a stroke) and constitutional symptoms (e.g. malaise, fatigue, weight loss) 1. left ventricle 2. interventricular septum 3. right atrium 4 left atrium 5 interatrial septum 6 tumor in the left atrium 2 Courtesy of Dr. Ketikoglou Dimitrios, Cardiologist MD PhD FESC
Is there any abnormality in this image of cardiac magnetic resonance imaging (MRI)?
Name the structures shown in the image.
There is a large intracavitary mass in the left ventricle in contact with the apical part of its lateral wall which has a morphology suggestive of a cardiac tumor. The mass is homogeneous, broad-based and well circumscribed. 1. left ventricle 2 interventricular septum 3 right ventricle 4 tumor in the left ventricle 5 left atrium 6 mitral valve 7 right atrium. 8 intratrial septum 9 left lung 10 right lung. 11 descending aorta. The mass was surgically excised and histologic examination showed that it was a lipoma (left ventricular lipoma) Note that transverse sections in MRI or CT are displayed as if the viewer looks at the patient from the patient's feet, so that the left-sided structures are seen on the right side of the image , the right-sided structures on the left side of the image, the anterior structures are seen on the top of the image and the posterior structures on the bottom. Courtesy of Dr. Ketikoglou Dimitrios, Cardiologist MD PhD FESC
-------------------------------------------------------------------------------------------------------------------------
A patient with hepatic cancer. What kind of view is this, how is it obtained, which are the structures 1-6 and what is the probable diagnosis for this patient ?
This is a transesophageal echocardiographic (TEE) bicaval view (a long axis view of the right atrium obtained from the middle esophageal position with a plane angle of about 90-100oand clockwise rotation of the transducer shaft). 1 left atrium 2 interatrial septum 3 entrance of the superior vena cava, 4 right atrium 5 entrance of the inferior vena cava 6 a large non-homogeneous mass in the right atrium with a morphology suggestive of a tumor. It is a metastatic tumor from the liver (as suggested by the patient's history which has metastasized through a hepatic vein and then through the inferior vena cava into the right atrial cavity. Courtesy of Dr. Ketikoglou Dimitrios, Cardiologist MD PhD FESC
A 3-D echocardiographic image. Which view is this and where is the abnormality ? Name possible symptoms that may result from such a pathology.
An apical 4-chamber 3-dimensional echocardiographic view showing a mass (tumor) in the left atrium. This was a rare case of metastasis of a tumor of the small intestine. A tumor in the left atrium can cause dyspnea (due to elevated left atrial and pulmonary venous pressure), syncope, arterial embolism (e.g. a stroke) and constitutional symptoms (e.g. malaise, fatigue, weight loss) 1. left ventricle 2. interventricular septum 3. right atrium 4 left atrium 5 interatrial septum 6 tumor in the left atrium 2 Courtesy of Dr. Ketikoglou Dimitrios, Cardiologist MD PhD FESC
Cardiac myxoma
Myxomas are the most common benign cardiac tumors in adults. A myxoma is an intracavitary mass, usually 4 -8 cm in diameter. In most cases, it is located in the left atrium (75%), attached to the interatrial septum, over the foramen ovale. More rarely, it is found in the right atrium and even less commonly in the ventricles. Most myxomas are sporadic (>90%) and seldom reoccur after complete resection. Multiple myxomas (synchronous, successive, or recurrent) are a feature of the myxoma syndromes (which account for 7% of cardiac myxoma cases). These cases are familial, as part of the rare Carney syndrome, which is a combination of cardiac and cutaneous myxomas, endocrine disorders (pituitary adenomas, adrenocortical disease, or testicular tumors), and cutaneous lentiginosis. (Lentiginosis is the presence of multple lentigines, i.e. small pigmented spots on the skin with a clearly defined edge, due to a benign hyperplasia of melanocytes which is linear in its spread)
When a familial myxoma syndrome is identified or suspected, screening first-degree relatives with echocardiography is mandatory.
When a familial myxoma syndrome is identified or suspected, screening first-degree relatives with echocardiography is mandatory.
Large myxomas are often mobile. They may move back and forth into the mitral valve annulus during a cardiac cycle.
Histologically, myxomas are neoplasms of multipotent mesenchymal cells in the subendocardial tissue. These are polygonal, occasionally multinucleate cells surrounded by a myxoid stroma.
A cardiac myxoma may induce constitutional symptoms (fever and weight loss) due to the production of interleukin-6, embolic phenomena, that can mimic systemic vasculitis or infective endocarditis and symptoms due to valvular obstruction (often mimicking mitral stenosis). Presenting symptoms of left-sided myxomas are dyspnea on exertion, paroxysmal nocturnal dyspnea, fever, and syncope. Sudden death may also occur. The most common physical finding with a myxoma of the left atrium is a mitral diastolic murmur (similar to mitral stenosis but without the opening snap) or an apical systolic murmur due to mitral incompetence. Occasionally there is an additional heart sound called tumor plop. This is an early diastolic sound. Raynaud phenomenon or clubbing of the fingers may occasionally occur.
On echocardiography, a myxoma has the appearance of a heterogeneous mobile mass, often globular, usually with a smooth or lobulated surface, 4-8 cm in diameter, attached to the endocardial surface (usually the interatrial septum) with a narrow base (stalk or pedicle). Occasionally it is attached with a wide base. Their echogenicity is not homogeneous and they may include areas of echolucensy and in some cases calcifications. Polypoid myxomas are larger with a smooth surface and they include lucencies and cystic areas due to hemorrhage and necrosis. Papillary myxomas tend to be smaller and have multiple villi. This subtype is associated with embolic phenomena,
On echocardiography, a myxoma has the appearance of a heterogeneous mobile mass, often globular, usually with a smooth or lobulated surface, 4-8 cm in diameter, attached to the endocardial surface (usually the interatrial septum) with a narrow base (stalk or pedicle). Occasionally it is attached with a wide base. Their echogenicity is not homogeneous and they may include areas of echolucensy and in some cases calcifications. Polypoid myxomas are larger with a smooth surface and they include lucencies and cystic areas due to hemorrhage and necrosis. Papillary myxomas tend to be smaller and have multiple villi. This subtype is associated with embolic phenomena,
The treatment of a cardiac myxoma is surgical resection of the tumor.
A transesophageal echocardiographic (TEE) image of a patient with exertional dyspnea and an episode of syncope. What kind of a TEE section is shown here, how is it obtained, which are the structures 1-9 and what is the diagnosis?
It is a TEE 5 chamber view obtained from the middle part of the esophagus (midesophageal 5 chamber view) with the image plane at 0o
A transesophageal echocardiographic (TEE) image of a patient with exertional dyspnea and an episode of syncope. What kind of a TEE section is shown here, how is it obtained, which are the structures 1-9 and what is the diagnosis?
It is a TEE 5 chamber view obtained from the middle part of the esophagus (midesophageal 5 chamber view) with the image plane at 0o
Other benign cardiac tumors: Lipoma / Papillary fibroelastoma (endocardial papilloma)
Lipomas result from a benign neoplastic proliferation of mature adipocytes and they are usually enclosed in a capsule in contrast to lipomatous hypertrophy (which is a condition that affects the interatrial septum). The majority of cardiac lipomas arise in the subepicardium, but occasionally they can be located in the pericardium, in the subendocardium, in the myocardium (intramural) or on the cardiac valves. Their size usually ranges from a few to several centimeters. On echocardiography, they appear homogenous, broad-based, immobile and well circumscribed. Usually, lipomas are asymptomatic, but occasionally they cause arrhythmias, atrioventricular block, or valvular dysfunction. A subepicardial lipoma may compress a coronary artery resulting in ischemic chest pain. Excision may be required because of the progressive growth of lipomas, as well as the above potential manifestations,
Lipomatous hypertrophy of the interatrial septum is a prominent thickening of the septum due to the accumulation of adipose tissue. The proximal and distal portions of the atrial septum appear thickened, generally with sparing of the fossa ovalis. Lipomatous hypertrophy of the interatrial septum is not a true tumor. It is more common in obese elderly women. It may be associated with supraventricular arrhythmias.
Lipomatous hypertrophy of the interatrial septum is a prominent thickening of the septum due to the accumulation of adipose tissue. The proximal and distal portions of the atrial septum appear thickened, generally with sparing of the fossa ovalis. Lipomatous hypertrophy of the interatrial septum is not a true tumor. It is more common in obese elderly women. It may be associated with supraventricular arrhythmias.
 |
| Papillary fibroelastoma of the aortic valve |
Papillary fibroelastoma is a benign tumor arising from the cardiac valves. It is the most common tumor of the cardiac valves. The average patient age is 60 years. Its diameter is often < 1 cm, but it may reach 1-2 cm, it has a small stalk and a shape resembling a sea anemone, floating in the blood. On echocardiography, these benign tumors have a small size, with independent motion and attachment to an endocardial surface (of a valve) via a central pedicle. The tumor typically has frond-like arms (small finger-like projections) and its borders appear shimmering, due to the vibration at the tumor-blood interface. The most common location is the aortic valve, followed by the mitral valve and rarely the right-sided valves or even the mural, nonvalvular endocardium. ,Papillary fibroelastomas may cause valvular incompetence and thromboembolic complications. Thromboembolic complications may manifest as a transient ischaemic attack, a stroke, myocardial infarction, sudden death, syncope, blindness, or pulmonary embolism. If the tumor is located on the arterial side of the aortic valve, it may cause coronary obstruction.Surgical excision of the tumor is curative and it is a reasonable decision in symptomatic patients or when the tumor has been diagnosed incidentally in a preoperative evaluation before cardiac surgery for another reason.
A Video Papillary fibroelastoma in 2D (modified short- and long-axis views) and 3D-transesophageal echocardiography. by the You Tube channel CDT
Cardiac sarcoma
Sarcomas are the most common malignant primary cardiac tumors. Typical age of presentation is between 40 and 50 years. On echocardiography, they appear as a broad-based mass with heterogeneous echogenicity, usually in the right atrium. They may also appear in any cardiac chamber and they also often affect the pericardium, resulting in a pericardial effusion and pericardial chest pain. When located in a right cardiac chamber they can affect tricuspid valve function, produce clinical manifestations of right-sided heart failure and /or metastasize to the lungs. Hypoechogenic areas may indicate tumor necrosis. Differential diagnosis is with a myxoma. In contrast to a myxoma, sarcomas do not have a stalk. Sarcomas tend to have a rapid growth, obstructing blood flow. Treatment with surgical debulking of the tumor is occasionally performed.GO BACK TO THE HOME PAGE AND TABLE OF CONTENTS LINK :
CARDIOLOGY BOOK ONLINE-HOME PAGE AND TABLE OF CONTENTS
Bibliography and links
LINK Cardiac Tumors
Takahashi A, Otsuka H, Harada M. Multimodal Cardiovascular Imaging of Cardiac Tumors. 2015;2(1):61-67. http://dx.doi.org/10.17996/anc.02.01.61
Mankad R, Herrmann J. Cardiac tumors: echo assessment. Echo Res Pract 2015;3(4):R65-R77. http://dx.doi.org/10.1530/erp-16-0035
LINK Cardiac tumors: echo assessment
Yuan S-M, Shinfeld A, Lavee J, et al. Imaging morphology of cardiac tumours. Cardiol J 2009; 16:26-35.
Yuan S-M, Shinfeld A, Lavee J, et al. Imaging morphology of cardiac tumours. Cardiol J 2009; 16:26-35.





No comments:
Post a Comment